Interview with Dr Vandana V. Prakash & Dr Mary Abraham, Author of “Managing Chronic Pain”
Gain insights from Dr. Vandana V. Prakash & Dr. Mary Abraham, authors of "Managing Chronic Pain," as they discuss holistic pain management strategies.on Apr 02, 2024
.jpg)
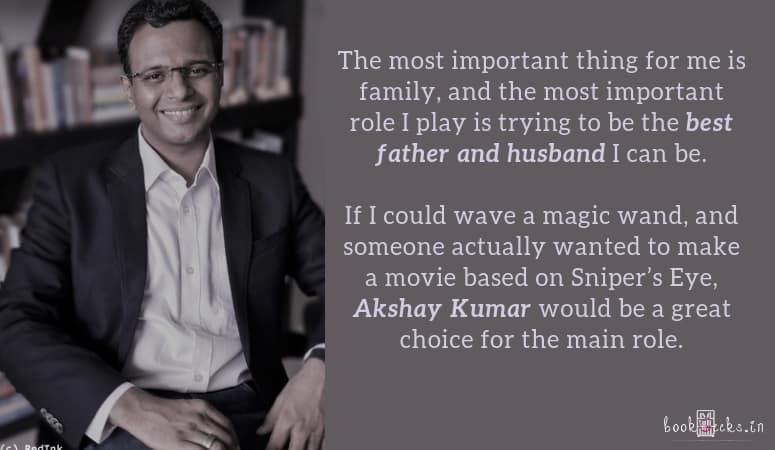
Dr Vandana V. Prakash is a senior consultant clinical psychologist practising for the past thirty years. She has an MPhil in medical and social psychology from NIMHANS, Bangalore. She has several research papers to her credit and has co-authored chapters on suicidal behaviour in adolescents for various international publications. She has also co-authored Conquering Pain (2019). Her next book is about learning disabilities. Dr Prakash is a clinician, researcher, academician and trainer.
Dr Mary Abraham is MD (AIIMS) and DNB anaesthesiology, with thirty-five years of experience in neuroanaesthesiology, pain and palliative care. She is a senior consultant in pain at the Max Multi Speciality Centre, Panchsheel Park, New Delhi. She has several papers to her credit, has contributed chapters in various books and has co-authored Conquering Pain (2019). She has organized many conferences and conducted workshops on neuroanaesthesia and pain medicine. She has contributed medical illustrations to various books, including Managing Chronic Pain. Dr Abraham is a clinician, researcher and academician.
Frontlist: Managing chronic pain involves understanding its multifaceted nature, including physical, emotional, and social dimensions. How do you navigate these complexities in your book to provide holistic insights for readers?
Dr Prakash & Dr Abraham: The pain that persists after twelve weeks, even when its protective role is over, and has lasted beyond the expected time of healing is termed chronic pain. Besides the unpleasantness of pain and the dysfunctionality it causes, when pain becomes chronic it tends to disrupt day-to-day life and brings in its wake many psychosocial issues. These could be anxiety, chronic low mood, depression, stress, occupational performance, change in dynamics of the house which affects relationship within the family and with the spouse. Due to the plethora of issues, thus created by chronic pain, often sufferers tend to distance themselves socially and emotionally and withdraw to themselves.
What may have started with only physical pain, subsequently with added psychosocial issues becomes a biopsychosocial experience. In this book, we have attempted to address not just the physical and biological consequences of chronic pain but also its psychological, social, and even spiritual ramifications. This is what is termed Total Pain and we have explained how this can affect the overall quality of life and how to manage it using a multimodal approach.
Frontlist: The mind-body connection is a central theme in your book. How do you explore this connection and its significance in the context of chronic pain management?
Dr Prakash & Dr Abraham: We have initially explained the biology and psychology of pain, including various models explaining the phenomenon. The risk factors, both modifiable and non-modifiable, physical, psychological, social, occupational, and cultural, have been described. The impact chronic pain has both on the mind and body of the person also constitutes a whole chapter. Once the expected problems have been identified, the holistic management of chronic pain has been addressed. We started the book with a case study and ended the book describing how various medical, physical, psychological, social, and occupational issues were addressed in that patient, using a combination of multi-modal treatment strategies by a multi-disciplinary team.
Frontlist: What are some common misconceptions about chronic pain that you aim to challenge or clarify through your book?
Dr Prakash & Dr Abraham: The most common myth about chronic pain is that it is purely physical pain gone awry and needs to be addressed only by medical specialists. However, chronic pain brings a plethora of psychological and social problems with it. If management is limited to only treating the physical pain, the relief thus obtained is also partial. Mind and particularly the emotional disturbances need to be addressed simultaneously to maximize the wellness quotient and have a more successful outcome.
Frontlist: As authors with extensive experience in clinical practice, research, and academia, how do you ensure that your insights are accessible and relevant to both medical professionals and general readers?
Dr Prakash & Dr Abraham: One of the reasons we wrote the book was to get a platform to reach a wider audience as interaction with patients alone is limited in its outreach experience. We were also aware of the huge number of persons who are suffering from chronic pain but have either no knowledge or only partial knowledge of the existence of pain specialists, pain clinics, and palliative care. Most persons especially in smaller towns and villages have no accessibility and means for the treatment of pain, whether it is chronic non-cancer or cancer pain. Although the biopsychosocial model has been prevalent in the western world, it is still in a nascent stage in our country. The biopsychosocial model of pain and its application in the holistic management of pain has been explained in a simple way that would be helpful to both non-medical and medical persons.
Frontlist: World Health Day emphasizes the importance of equity in healthcare. How does your book address disparities in chronic pain management and advocate for fairer access to effective treatments?
Dr Prakash & Dr Abraham: Pain, till a couple of decades back, was considered either an offshoot of a medical condition and/or an integral part of other specialties in medical science. Pain to be recognized as a special branch only happened with the declaration by the United States Congress proclaiming 2001–2010 as the ‘Decade of Pain Control and Research’. Nearly 20 percent of people worldwide suffer from chronic pain with serious ramifications in terms of mental health, occupational efficiency, and it is also a burden on the health exchequer. Chronic pain does not differentiate between social strata, age, or any other educational or economic factors but can affect anyone. Availability of treatment needs to be provided for all irrespective of these differences.
Unfortunately, equity in healthcare is not present in many countries worldwide. According to International Human Rights Law, countries have to provide pain relief to sufferers of pain as part of their core obligations under the right to health. In 2014, the World Health Assembly, the decision-making body of the WHO, passed a resolution that palliative care should be an integral part of healthcare. The WHO recommends that palliative should be integrated into the primary health care level so that all citizens can access it especially for cancer pain.
In this book we have elaborated on innumerable treatment strategies for managing chronic pain using the biopsychosocial approach. However, there should be enough trained medical professionals to carry out these treatment methods. One policy that can be adopted is making it mandatory for every hospital to have pain and palliative care clinics and to have awareness programs so that people from all walks of life know about the existence of these facilities.
Frontlist: Can you highlight some practical strategies or exercises from your book that individuals can incorporate into their daily lives to better manage chronic pain?
Dr Prakash & Dr Abraham: Prevention is always better than cure. One can prevent and manage chronic pain by implementing lifestyle changes as well as having routine medical checkups. Lifestyle changes include daily physical activity and exercise, good and healthy nutrition, controlling body weight, good work ergonomics, adequate sleep, control stress levels, and maintaining a good work-life balance. Regular health checkups can detect any deficiencies or comorbidities that may be present. The psychological aspects can be addressed by acceptance of the problem, willingness to deal with both the physical and emotional impact of chronic pain, pursuing one's cherished goals, and working on them to the best of one’s capacities, despite the presence of pain. Simple daily routines like yoga, meditation, incorporating dance, art, music therapies can easily be followed. For emotional release ventilation, externalization of interests, tension release through diary writing like emotional diary writing and pain diaries are helpful.
Frontlist: Chronic pain often affects not only the individual experiencing it but also their family, social relationships, and overall quality of life. How does your book address the broader impact of chronic pain on various aspects of well-being?
Dr Prakash & Dr Abraham: Family and social issues are a part of nearly all the chapters of the book. When a person is afflicted with chronic pain, the dynamics of the family changes. The healthier partner has to don the mantle of responsibilities for the family. The partner as well as a cohesive family who able to deal with changed circumstances would be able to have good spousal and familial relationships. The converse is equally true. The book also describes the hostility or expressed emotions that may develop within the spousal and familial relationships against the chronic pain patient. When we see the relationships being affected, marital therapy and family therapies are incorporated as part of the treatment program. We did it with Rahul’s spouse and the family when it became obvious that the angst within the family was becoming a deterrent in his overall improvement.
Frontlist: Lastly, what message or insight do you hope readers will take away from "Managing Chronic Pain," and how do you envision it contributing to a greater understanding and improvement in chronic pain management practices?
Dr Prakash & Dr Abraham: First and foremost, we hope that the readers understand the significance of the biopsychosocial phenomenon of chronic pain. The biology and psychology of chronic pain, risk factors both modifiable and non-modifiable, and the impact chronic pain has on the mind and body are precursors to seeking treatment. Targeting only physical pain in the absence of healing mental pain is a job half done. For example, if a patient with chronic pain has major depression or chronic depression (dysthymia), the pain experience would not be alleviated by treating only the physical pain as one of the symptoms of depression is pain. Despite the best efforts of a pain specialist to treat physical pain, the patient would still feel pain if depression, anxiety, stress, unrefreshed sleep, obesity and so on are not simultaneously addressed. Chronic pain can and often does result in disabilities which adversely affect the quality of life of not only the patient but the partner, family, and extended social milieu. Recognizing and working upon these issues would help in a long way for better life adjustments and a better outcome.

.jpg)
.jpg)
.jpg)
.jpg)
.jpg)

.jpg)
.jpg)
.jpg)
.jpg)
.jpg)


.jpg)
.jpg)
_(1).jpg)
Sorry! No comment found for this post.